How Great Thou Art: A Comprehensive Guide to Sheet Music & Resources (Updated January 26, 2026)
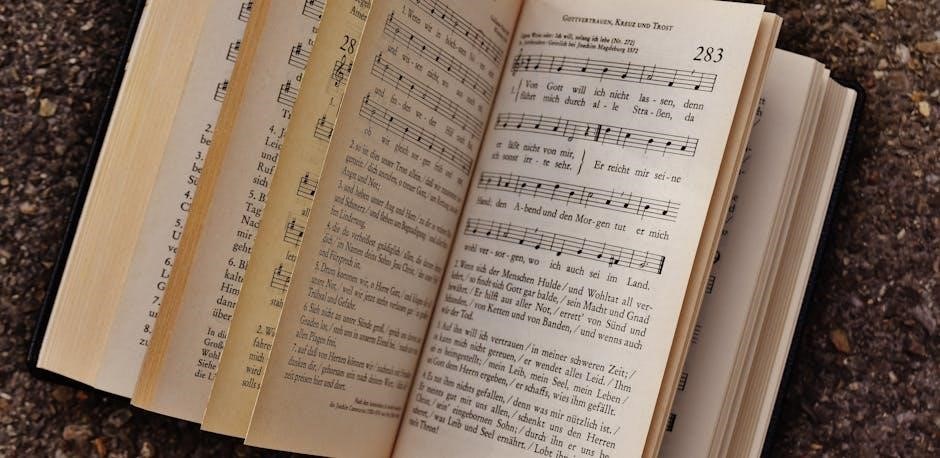
Discover readily available, free How Great Thou Art sheet music PDFs for piano, guitar, and flute, shared by a vast online community of musicians and creators.

“How Great Thou Art” transcends generations, remaining a cornerstone of Christian worship and a beloved hymn worldwide. Its powerful lyrics and soaring melody inspire reverence and praise.
The accessibility of sheet music PDFs has significantly contributed to its continued popularity, allowing musicians of all levels to learn and perform this timeless classic.
From simple piano arrangements to complex choral scores, the availability of free and paid resources online ensures the hymn’s enduring legacy.

This guide explores the wealth of sheet music options, empowering you to experience and share the beauty of “How Great Thou Art”.
Historical Background of the Hymn
“How Great Thou Art” began as a Swedish poem, “O Store Gud” (“O Great God”), penned by Carl Boberg in 1898 after a powerful spiritual experience. The hymn’s journey to global recognition was facilitated by translations, notably into English.
The widespread distribution of sheet music, initially in its original Swedish and then English forms, played a crucial role in its dissemination.
Today, the ease of accessing sheet music PDFs online continues this tradition, allowing musicians to connect with the hymn’s rich history and profound message.

Understanding its origins enhances appreciation for this enduring piece of sacred music.
Origins in Swedish Hymnody
“How Great Thou Art” traces its roots to 1898 Sweden, born from Carl Boberg’s poem, “O Store Gud.” Inspired by a powerful sunset and a profound sense of God’s majesty, Boberg’s verses quickly resonated within Swedish Christian communities.
Early dissemination relied on printed sheet music, spreading the hymn’s message through churches and homes. The availability of this sheet music, even in its initial form, was vital.
The hymn’s Swedish origins highlight a rich tradition of devotional songwriting, paving the way for its eventual global impact, now easily accessible via PDF versions online.
Carl Boberg’s Inspiration & Initial Composition
In 1898, Carl Boberg, a Swedish lay preacher, penned the original lyrics after witnessing a breathtaking sunset while walking home from an evening service. This experience ignited a powerful reflection on God’s creation and boundless power.
Initially, Boberg’s work was a poem, not a song. Later, he set it to a traditional Swedish melody. Early sheet music reflected this pairing, though variations existed. The availability of this initial sheet music was crucial for its spread.
Boberg’s heartfelt composition, now widely available as a PDF, continues to inspire reverence and praise globally.
Translation into English
The hymn’s journey to global recognition hinged on its English translation. Several attempts were made, but the version by Clarence Walworth, in 1925, became definitive. This translation preserved the poem’s emotional depth and theological richness.
Walworth’s English lyrics, paired with a Russian melody, created the version we know today. Early English sheet music editions featured this combination, becoming increasingly popular. Finding a reliable PDF of this version is now simple.
The translated sheet music facilitated the hymn’s adoption across denominations and cultures.
Finding “How Great Thou Art” Sheet Music PDF Online
Locating “How Great Thou Art” sheet music PDF versions is remarkably easy thanks to numerous online resources. Websites like 8notes.com offer free and paid arrangements for various instruments. A quick search reveals a wealth of options, catering to different skill levels.
Many sites provide downloadable PDFs, perfect for immediate use. However, always verify the legality and copyright status before downloading. Explore curated lists featuring multiple arrangements, ensuring you find the perfect fit for your needs.
Digital music libraries are brimming with this beloved hymn.
Popular Sheet Music Websites (8notes, etc.)
Several prominent websites specialize in providing sheet music PDFs, including “How Great Thou Art.” 8notes.com stands out, offering both free and premium arrangements for piano and other instruments. Musicnotes.com and SheetMusicPlus are also excellent resources, though typically requiring a purchase.
These platforms boast extensive catalogs and user-friendly interfaces. Many allow you to preview the music before downloading. Explore options for transposing the key or adjusting the arrangement to suit your preferences. Remember to check user reviews for quality assessments.
Free vs. Paid Sheet Music Options
Numerous websites offer free “How Great Thou Art” sheet music PDFs, often community-submitted, but quality can vary. These are ideal for beginners or casual players. Paid options, available on sites like Musicnotes.com and SheetMusicPlus, generally provide higher-quality, professionally arranged music.

Paid versions often include accurate transcriptions, clean layouts, and may offer accompaniments or arrangements for different instruments. Consider your skill level and desired arrangement when choosing. Free options are great for practice, while paid versions are suitable for performance or serious study.
Legality and Copyright Considerations
Downloading sheet music raises copyright concerns. While many older hymns like “How Great Thou Art” are in the public domain, specific arrangements may still be protected. Free PDF downloads from unofficial sources could infringe on copyright.
Reputable sheet music websites typically secure licenses or offer public domain arrangements legally. Always check the terms of use before downloading and using any sheet music. Supporting copyright holders ensures continued creation of quality arrangements. Using legally obtained music protects both you and the composer’s rights.
Sheet Music Arrangements for Different Instruments
Numerous arrangements of “How Great Thou Art” exist for diverse instruments. Piano sheet music ranges from beginner-friendly simplified versions to complex, advanced arrangements. Guitarists can find chord charts, tablature, and intricate fingerstyle arrangements.
Vocal arrangements cater to soloists and SATB choirs, offering harmonies and accompaniment. Beyond these, sheet music is available for instruments like flute and violin, expanding performance possibilities. Finding the right arrangement depends on skill level and desired instrumentation, with many PDF options readily accessible online.
Piano Arrangements: Beginner, Intermediate, Advanced
Piano sheet music for “How Great Thou Art” spans all skill levels. Beginner arrangements simplify the hymn, focusing on basic chords and melodies, ideal for early learners. Intermediate versions introduce more complex harmonies and rhythms, building upon foundational skills.
Advanced arrangements offer elaborate embellishments, intricate voicings, and challenging passages for experienced pianists. Many free PDF options are available online, alongside paid, professionally arranged sheet music offering higher fidelity and detailed notation. Choose based on your proficiency and musical goals.
Guitar Arrangements: Chords, Tabs, Fingerstyle
Guitarists can find “How Great Thou Art” sheet music in various formats. Chord charts provide simplified accompaniment for strumming, perfect for group singing. Tablature (tabs) displays finger placement, enabling easier learning of melodies and riffs.
Fingerstyle arrangements offer a more intricate and expressive approach, utilizing individual string picking. Numerous free PDF resources exist online, catering to different skill levels. Paid options often include detailed transcriptions and performance notes, enhancing the learning experience for dedicated guitarists.
Vocal Arrangements: Solo, SATB Choir
Vocalists seeking sheet music will discover options for both solo performance and choir arrangements. Solo sheets typically feature melody lines with piano accompaniment, ideal for individual practice or worship leading. SATB (Soprano, Alto, Tenor, Bass) arrangements are designed for four-part choral singing, commonly used in church settings.
Many free PDF resources provide lead sheets, while more elaborate choral scores are often available for purchase. These often include harmonies and dynamic markings, enriching the vocal experience and facilitating beautiful ensemble performances.
Other Instrument Arrangements (Flute, Violin, etc.)
Beyond piano and guitar, sheet music PDFs for “How Great Thou Art” extend to instruments like flute and violin, broadening performance possibilities. These arrangements often adapt the melody for single-instrument performance, sometimes including a piano accompaniment track.
Finding these resources requires dedicated searching on sheet music websites. While less common than piano or vocal arrangements, dedicated musicians can locate suitable scores for various instruments, allowing for unique and expressive interpretations of this beloved hymn. Explore to enrich your musical repertoire!

Understanding Sheet Music Notation
Decoding “How Great Thou Art” sheet music PDFs requires familiarity with musical notation basics. Key signatures indicate sharps or flats, defining the tonal center, while time signatures dictate rhythm.
Successfully reading notes and understanding their rhythmic values is crucial. Dynamic markings (p for piano, f for forte) control volume, and articulation symbols (staccato, legato) shape phrasing. Mastering these elements unlocks the hymn’s expressive potential, allowing musicians to accurately interpret and beautifully perform the piece.
Key Signatures and Time Signatures
Analyzing “How Great Thou Art” sheet music PDFs begins with understanding key and time signatures. Commonly, arrangements appear in G major, indicated by one sharp in the key signature. This impacts note reading.
The time signature is typically 4/4, meaning four beats per measure, with a quarter note receiving one beat. Recognizing these foundational elements is vital for accurate rhythm and tempo. These signatures establish the harmonic and rhythmic framework, enabling musicians to confidently navigate and perform the hymn’s beautiful melody.
Reading Notes and Rhythms
Successfully interpreting “How Great Thou Art” sheet music PDFs requires proficient note and rhythm reading. The melody primarily utilizes notes within a comfortable range for most vocalists and instrumentalists. Pay close attention to note durations – whole, half, quarter, and eighth notes – to maintain accurate timing.
Rests are equally important! Understanding their values ensures proper phrasing and musicality. Practice slowly, focusing on precise note execution and rhythmic accuracy. Consistent practice builds fluency, allowing for a more expressive and heartfelt performance of this beloved hymn.
Dynamic Markings and Articulation
Enhance your performance of “How Great Thou Art” sheet music PDFs by carefully observing dynamic markings – piano (soft), mezzo forte (medium loud), and forte (loud) – which shape the emotional impact. Articulation marks, like staccato (short, detached) and legato (smooth, connected), further refine expression.
These nuances guide phrasing and intensity. A gradual crescendo builds towards powerful climaxes, while diminuendos create moments of reverence. Paying attention to these details transforms a simple reading into a deeply moving interpretation of this timeless hymn, conveying its profound message.
Printing and Using Sheet Music PDFs
Successfully utilizing “How Great Thou Art” sheet music PDFs begins with optimal print settings. Select “Fit to Page” to avoid cropping notes, ensuring clarity. Preview before printing! Utilize PDF viewing software like Adobe Acrobat Reader for easy navigation and annotation.
When practicing, consider using a tablet for portability and adjustable lighting. Mark phrasing and dynamics directly on the PDF for personalized study. Consistent practice with a clearly printed or digitally displayed score will unlock a beautiful rendition of this beloved hymn.
Optimal Print Settings for Clarity
Achieving a clear print of your “How Great Thou Art” sheet music PDF is crucial. Select your printer’s “Best” quality setting for sharp notation. Choose “Fit to Page” scaling to prevent any musical elements from being cut off, especially ledger lines.
Always preview the print before committing to paper! Ensure the key signature and time signature are fully visible. A grayscale print can conserve ink while maintaining readability. Experiment with margins to maximize space without sacrificing clarity – a well-printed score enhances practice.
Software for Viewing and Editing PDFs
Numerous software options enhance your “How Great Thou Art” sheet music PDF experience. Adobe Acrobat Reader is a free, reliable viewer. For annotation and basic editing, consider PDFescape or Smallpdf online tools.

More advanced editing – like transposing or adding markings – requires paid software such as Adobe Acrobat Pro or Finale Notepad. These programs allow customization. Preview on Mac also offers basic PDF viewing and annotation. Ensure your chosen software supports high-resolution display for optimal readability of the hymn’s notation.
Tips for Practicing with Sheet Music
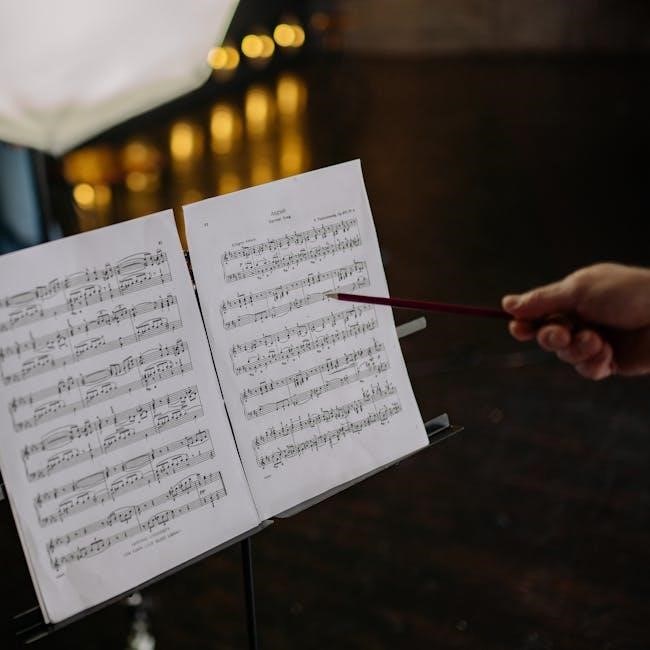
Effectively utilizing your “How Great Thou Art” sheet music PDF requires focused practice. Start slowly, mastering individual sections before combining them. Use a metronome to maintain consistent tempo.
Highlight difficult passages and practice them repeatedly. Consider playing along with recordings to internalize the melody and harmonies. Don’t hesitate to mark dynamics and articulation directly on the PDF for clarity. Regular, short practice sessions are more beneficial than infrequent, lengthy ones. Embrace patience and enjoy the beautiful hymn!
Variations and Different Versions of the Hymn
Exploring the diverse world of “How Great Thou Art” sheet music PDFs reveals fascinating variations. Different English translations exist, subtly altering lyrical phrasing and impacting musical interpretation.
Many arrangements feature added introductions or endings, enhancing the hymn’s dramatic effect. Contemporary interpretations may incorporate modern harmonies or instrumentation. When comparing PDFs, note differences in key signatures and vocal arrangements (solo, SATB). These variations offer opportunities to personalize your performance and deepen your appreciation for this timeless classic.
Comparing Different English Translations
Analyzing various “How Great Thou Art” sheet music PDFs highlights the nuances of English translations. While conveying the same core message, lyrical choices differ, impacting phrasing and emotional resonance. Some translations prioritize literal accuracy, while others emphasize poetic flow.
These subtle shifts influence musical interpretation and vocal delivery. Comparing PDFs side-by-side reveals these differences, allowing musicians to select a version aligning with their artistic vision. Consider how each translation affects the hymn’s overall impact and choose the one that best resonates with your performance style.
Exploring “How Great Thou Art” sheet music PDFs often reveals arrangements extending beyond the original hymn structure. Many composers add instrumental introductions, building anticipation and establishing the hymn’s majestic tone. Similarly, extended endings, featuring harmonic variations or instrumental flourishes, provide a powerful conclusion.
These additions enhance the musical experience, offering opportunities for dynamic expression and showcasing instrumental skill. When selecting a PDF, consider whether these embellishments suit your performance context and musical preferences. They can elevate the hymn’s impact, but also require additional practice.
Contemporary Interpretations of the Hymn
Modern “How Great Thou Art” sheet music PDFs showcase diverse interpretations, moving beyond traditional arrangements. Contemporary versions often incorporate stylistic elements from genres like gospel, pop, or even cinematic orchestration. These arrangements frequently feature altered harmonies, rhythmic variations, and dynamic shifts to resonate with modern audiences.
Some PDFs include simplified chord progressions for easier accompaniment, while others present complex arrangements for advanced musicians. Exploring these interpretations reveals the hymn’s adaptability and enduring appeal. Consider the arrangement’s style when selecting a PDF, ensuring it aligns with your musical vision and performance goals.
Resources for Learning to Play “How Great Thou Art”
Numerous online tutorials and video lessons accompany “How Great Thou Art” sheet music PDFs, catering to various skill levels. Many websites offer sheet music with embedded audio, allowing learners to hear correct phrasing and timing. Platforms like YouTube host countless performances and instructional videos, providing visual guidance.
For personalized instruction, consider local music teachers specializing in hymns or gospel music. Workshops focused on hymn playing can also accelerate learning. Utilizing these resources alongside your chosen PDF will enhance your understanding and performance of this beloved hymn.
Online Tutorials and Video Lessons
YouTube is a treasure trove of “How Great Thou Art” tutorials, ranging from beginner piano lessons using the sheet music PDF to advanced vocal arrangements. Many instructors break down the hymn into manageable sections, focusing on chords, melodies, and rhythms.
Websites dedicated to music education also provide structured courses. Search for “How Great Thou Art piano tutorial PDF” or “guitar lesson sheet music” to find targeted resources. These lessons often complement the sheet music, offering visual and auditory learning aids for a comprehensive experience.
Sheet Music with Embedded Audio
Several platforms offer “How Great Thou Art” sheet music PDFs integrated with audio playback features. This allows musicians to hear the correct tempo, phrasing, and articulation while following along with the notation. 8notes.com, for example, provides some arrangements with this functionality, enhancing the learning process.
These interactive scores are particularly beneficial for beginners, aiding in accurate interpretation. The audio component bridges the gap between seeing the notes on the page and hearing the intended sound, fostering a deeper understanding of the hymn’s musicality and improving practice efficiency.
Local Music Teachers and Workshops
Supplementing online resources, consider lessons with a local music teacher specializing in hymns or sacred music. A teacher can provide personalized guidance on interpreting “How Great Thou Art” sheet music, focusing on technique and musical expression. Workshops centered around hymn playing are also valuable.
These often cover topics like harmonization, accompaniment styles, and congregational leading. A skilled instructor can help navigate challenging passages and offer insights into the hymn’s historical and theological context, enriching your understanding beyond simply reading the PDF.
“How Great Thou Art” in Worship and Church Settings
Churches frequently utilize “How Great Thou Art” sheet music for worship services, often employing arrangements suitable for congregational singing or special performances. Having readily accessible PDF versions simplifies preparation for pianists, organists, and vocal leaders.
Church musicians can adapt sheet music to various instrumental combinations, ensuring a rich and engaging experience for the congregation. Utilizing clear, well-printed PDFs minimizes errors during services, fostering a more reverent atmosphere. The hymn’s enduring popularity makes it a staple in many Christian traditions.
Its Role in Christian Liturgy
“How Great Thou Art” frequently appears within Christian liturgy as a powerful expression of praise and adoration. Sheet music PDFs enable worship leaders to seamlessly integrate the hymn into various service elements, from offertory pieces to closing hymns.
The hymn’s theological depth resonates with core Christian beliefs, making it suitable for significant liturgical seasons. Access to accurate sheet music ensures faithful reproduction of the melody and harmony, enhancing the communal worship experience. Utilizing readily available PDFs streamlines musical preparation for church services.
Accompaniment Options for Congregational Singing
Sheet music PDFs of “How Great Thou Art” facilitate diverse accompaniment styles for congregational singing. Simple piano arrangements, easily sourced online, are ideal for smaller churches or less experienced musicians. Guitar chord charts, also widely available as PDFs, offer a more informal, accessible option.
More elaborate arrangements, featuring richer harmonies and instrumental parts, can elevate the worship experience. Utilizing these PDFs allows worship teams to tailor the accompaniment to their specific skills and resources, fostering enthusiastic participation from the entire congregation.
Using Sheet Music for Church Musicians
Church musicians benefit greatly from accessing “How Great Thou Art” sheet music PDFs in various arrangements. Vocalists can utilize solo arrangements to prepare performances, while choir directors can leverage SATB scores for harmonious ensemble singing.
Instrumentalists find PDFs invaluable for practicing accompaniment parts – piano, guitar, or even flute/violin arrangements. These resources allow for customized arrangements, adapting to the church’s musical style and available talent. PDF format enables easy printing, annotation, and sharing amongst the worship team, streamlining rehearsal processes.
Related Hymns and Songs
Exploring hymns sharing similar themes of praise and awe with “How Great Thou Art” enriches musical understanding. Consider “Holy, Holy, Holy! Lord God Almighty” or “A Mighty Fortress Is Our God,” both expressing profound reverence.
Numerous songs draw inspiration from this classic hymn, echoing its message of divine majesty. Discovering these connections expands the repertoire for worship leaders and musicians. Accessing sheet music PDFs for these related pieces allows for seamless integration into services, fostering a continuous flow of adoration and spiritual reflection within the congregation.
Hymns with Similar Themes of Praise and Awe
Delving into hymns that mirror the profound praise and awe found in “How Great Thou Art” reveals a rich tapestry of worship music. “Holy, Holy, Holy! Lord God Almighty” powerfully proclaims God’s holiness, while “A Mighty Fortress Is Our God” celebrates divine protection.
Finding sheet music PDFs for these related hymns allows musicians to build a cohesive worship set. Exploring arrangements for piano, guitar, or choir enhances the experience. These selections, like “Be Thou My Vision,” share a similar emotional depth, fostering a spirit of reverence and gratitude within the congregation.
Songs Inspired by “How Great Thou Art”
Numerous contemporary Christian songs draw inspiration from the majestic themes of “How Great Thou Art,” echoing its message of divine grandeur. Artists have subtly incorporated melodic fragments or lyrical concepts, creating new expressions of faith.
Accessing sheet music PDFs of these inspired songs alongside the original hymn provides a fascinating study in musical evolution. Many arrangements are available for various instruments, facilitating diverse worship styles. Exploring these connections deepens appreciation for the hymn’s enduring influence on modern Christian music, showcasing its lasting legacy.
Exploring the Wider Repertoire of Christian Hymns
Delving into the broader world of Christian hymnody reveals a rich tapestry of praise and worship. Many hymns share thematic similarities with “How Great Thou Art,” focusing on God’s power and creation’s beauty.

Finding sheet music PDFs for these related hymns – like “Amazing Grace” or “Holy, Holy, Holy!” – expands a musician’s repertoire and understanding of the genre. This exploration fosters a deeper connection to the historical and theological roots of Christian music, enriching both personal devotion and communal worship experiences.